Abstract
An anatomical variant of the Stafne bone cavity (SBC) located in the right subcondylar region of the mandible is presented. Such an occurrence of the SBC in this region near the parotid gland is considered rare and poses a diagnostic challenge for the dentist and radiologist. Knowledge of head and neck clinical anatomy and imaging studies such as plain film panoramic radiographs and cone beam CT scans can assist the clinician in arriving at a correct definitive diagnosis without surgical intervention.
Author Contributions
Academic Editor: Pietro Scicchitano, Cardiology Department, Hospital of Ostuni (BR) - Italy.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2019 Cameron Y. S. Lee, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Stafne bone cavity (SBC) is classically described as an asymptomatic depression or concavity localized on the medial surface of the posterior mandible between the inferior alveolar canal and inferior border.1It is considered a pseudocyst as the lesion does not have an epithelial lining. Although the exact morphogenesis is not known, it is hypothesized that during embryological development of the mandible from Meckel’s cartilage, the submandibular gland tissue is entrapped that leads to an osseous concavity on the medial surface of the mandible. 1,2
Radiographic features (Figure 1) of the SBC are a well-circumscribed unilocular, round or elliptical shaped radiolucency in the posterior mandible that are approximately 10 to 30mm in length. 1,3,4The radiographic lesion is often incidentally discovered when the patient completes a routine panoramic radiograph at the dentist office and does create concern for the dentist as it can mimic a cystic lesion.3,5,6
Figure 1.Panoramic radiograph of classically described SBC of the right posterior mandible illustrates the well-defined unilocular radiolucency in the right posterior mandible between the inferior alveolar canal and the inferior border of the mandible (arrows).
As patients are asymptomatic, the SBC can be difficult to diagnosis when the lesion is localized to a different anatomic part of the mandible. Although the most common location is the medial surface of the posterior mandible in the region of the submandibular gland fossa,1,3,4Philipsen et al (2002) described four variants of the SBC based on anatomic location of the mandible. The most common location is the medial surface of the posterior mandible from the first molar to the angle. Less common occurrences are on the medial and lateral surfaces of the ramus of the mandible. An atypical location of the radiolucent bone lesion other than the posterior mandible on a panoramic radiograph can raise concern and present a diagnostic challenge to the dentist or even the radiologist regarding osseous pathology. The incidence of the SBC has been reported to range from 0.1 to 6.06%.7
The goal of this case report is to present a variant of the Stafne bone cavity localized to the medial surface of the right subcondylar neck of the mandible in our patient discovered during completion of a routine panoramic radiograph.
Case Report
A 63-year old asymptomatic Asian male presented to the office upon referral from his dentist for evaluation of a radiolucent lesion in the right subcondylar neck of the mandible. The patient stated that the radiographic lesion was incidentally discovered when the panoramic radiograph was completed at his last routine annual dental examination. The patient’s medical history was significant for hypertension. Current medications prescribed by his physician consisted of metoprolol XL, 200mg and Lipitor 40mg, daily. No history of malignancy was reported by the patient.
Maxillofacial examination was unremarkable. No facial swelling, masses or asymmetry was observed. The TMJ examination was normal. No pain or tenderness to digital palpation was observed in the right preauricular region. Oral examination of the patient was unremarkable. No trismus was observed as the maximal interincisive opening was greater than 40.0mm. No anterior or posterior open bite was observed. Imagining studies to rule-out intraosseous neoplastic lesions and arrive at a definitive diagnosis consisted of a panoramic radiograph and cone beam CT scan (120 kVp, 5 mA, 7.4 sec). Panoramic radiograph revealed a unilocular, well-circumscribed radiolucency in the right subcondyalar region of the mandible that was close to the posterior border of the condylar neck (Figure 2). Cone beam CT scan (i-CAT FLX, Imaging Sciences, Hatfield, PA) imaging revealed a well-defined unilocular, elliptical shaped radiolucent lesion on the medial surface of the right subcondylar neck of the mandible (Figure 3, Figure 4, Figure 5). The elliptical shaped unilocular lesion involved almost the entire horizontal dimension of the subcondylar neck (Figure 4). Figure 5 shows the three-dimensional CT scan reconstruction (i-CAT FLX, Imaging Sciences, Hatfield, PA) of the medial defect in the subcondylar region of the mandible. Based on knowledge of clinical head and neck anatomy and imaging studies, no treatment was indicated as the diagnosis was consistent with a variant of a Stafne bone cavity of the right subcondylar neck near the parotid gland and not a pathological condition. The patient was informed about the risk of condylar neck fracture due to the critical size of the SBC.
Figure 2.Panoramic radiograph reveals a unilocular radiolucency in the right subcondylar neck of the mandible which is considered a variant of the classic SBC described by Dr. Stafne.
Figure 3.Axial cone beam CT scan showing osseous bone defect with herniation of soft tissue in the medial cortex of the right subcondylar neck of the mandible.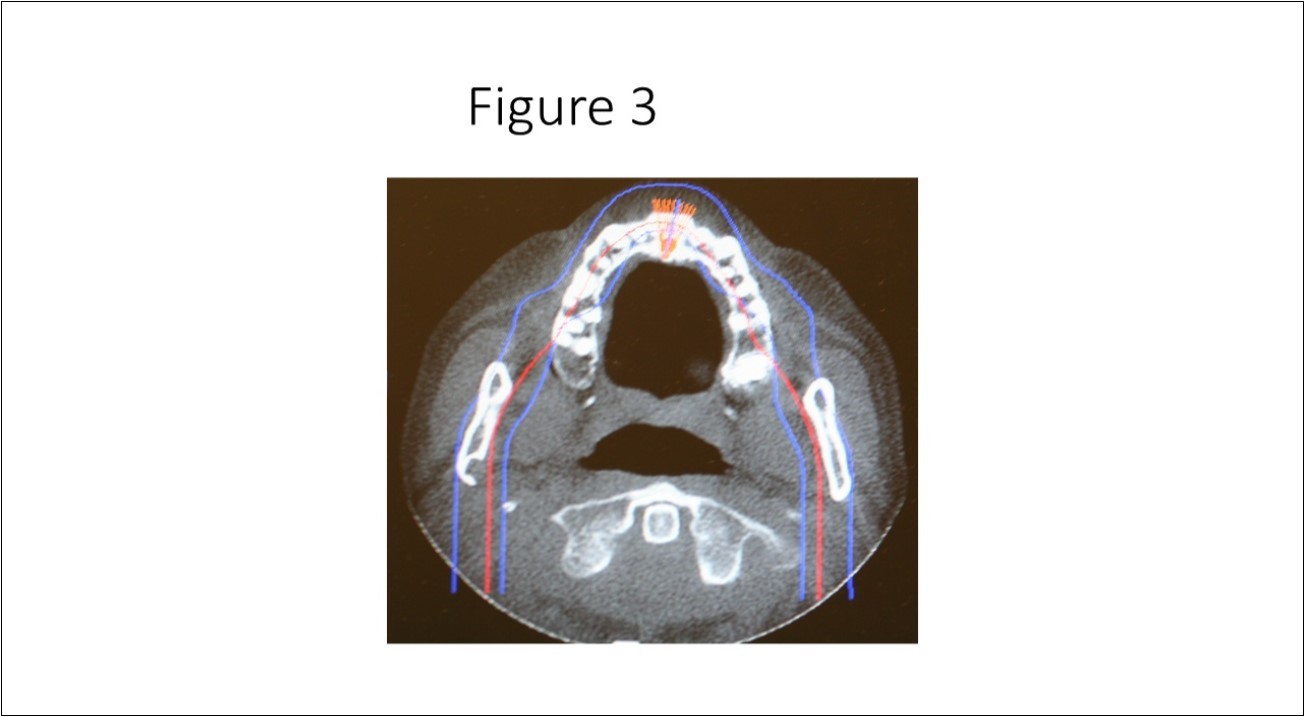
Figure 4.Cone beam CT TMJ sagittal views illustrate osseous defect on medial cortex. Note the thinness of the cortex that places the patient at risk for fracture of the condylar neck.
Figure 5A.Three-dimensional cone beam CT scan reconstruction revealing osseous defect in medial cortex of right subcondylar neck of mandible.
Figure 5B.Three-dimensional cone beam CT scan close up view of osseous defect on medial cortex of right subcondylar neck of mandible.
Discussion
Definitive diagnosis of SBC is made by imaging studies as they provide accurate anatomic information without surgical intervention. Radiographically, the Stafne bone cavity is usually observed between the inferior alveolar canal and inferior border of the posterior mandible from the ramus to the premolar regions on a panoramic radiograph.3,4,5,6However, there are variances in the location of the SBC. An atypical variant in the subcondylar region of the mandible near the parotid gland was first reported by Wolf 9and later Barker.10Both authors described the variant as a “parotid or ramus” variant of the Stafne bone cavity. In 2004, Campos et al 11using cone beam CT scan technology reported a parotid gland variant of the SBC as a salivary gland defect. They hypothesized that the osseous concavity was due to failure of ossification of the mandible and not the salivary gland.
Stafne bone cavity located in the subcondylar region of the mandible is considered a rare variant of the well-described SBC in the mandibular posterior mandible first reported by Stafne in 1942. There is a paucity of published case reports of SBC identified in the subcondylar or ascending ramus of the mandible in the English world medical and dental literature.9,19In a study by Sisman et al 3using computed tomography they concluded that the SBC is due to the presence of aberrant submandibular gland tissue within the osseous defect on the medial surface of the mandible. As it is hypothesized that the submandibular gland tissue is entrapped that leads to an osseous concavity on the medial surface of the mandible, it is also plausible that the parenchymal tissues of the parotid gland can also become entrapped in the developing mandible that leads to a similar osseous concavity (Figure 3) in the subcondylar region of the mandible.20
Intraosseous radiolucencies observed in the subcondylar region of the mandible are rarely observed radiographically. For the clinician, identification of and diagnosis of such lesions is often challenging. The differential diagnosis of SBC may include the following: odontogenic cyst, aneurysmal bone cyst, traumatic bone cyst, osteoporotic bone marrow defect, ameloblastoma, myxoma, hemangioma, multiple myeloma, giant cell tumor and metastatic disease.5,21,22However, deposition of fat, vascular, and salivary glandular tissue herniated into the osseous concavity should also be considered in the differential diagnosis. In our case report, based on the anatomic location, imaging findings, a normal examination in our asymptomatic patient, the diagnosis was consistent with a rare variant of the SBC localized to the subcondylar region of the mandible. No treatment is indicated for this anatomic variant of the SBC. However, when the diagnosis is uncertain, magnetic resonance imaging and biopsy should be considered.3,20,21
Conclusion
An anatomical variant of the Stafne bone cavity (SBC) located in the right subcondylar region of the mandible is considered rare and poses a diagnostic challenge for the clinician and radiologist. Knowledge of clinical anatomy, and imaging studies such as plain film panoramic radiographs and cone beam CT scan can assist the clinician in arriving at a correct definitive diagnosis without surgical intervention.
Author Disclosure
None Declared.
References
- 2.Carlson G. (2000) The salivary glands. Embryology, anatomy and surgical applications. Surg Clin North Am. 80, 261-273.
- 3.Sisman Y, Miloglu O, Sekerci A E. (2012) Radiographic evaluation on prevalence of Stafne bone defect: a study for two centres in Turkey. Dermatomaxillofacial Radiology. 41, 152-158.
- 4.Ariji E, Fujiwara N, Tabata O. (1993) Stafne’ s bone cavity. Classification based on outline and content determined by computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 76(3), 375-380.
- 5.Philipsen H P, Takata T, Reichart P A. (2002) Lingual and buccal mandibular bone depressions: a review based on 583 cases from a world-wide literature survey, including 69 new cases from Japan. Dentomaxillofac Radiol. 31(5), 281-90.
- 6.Tsui S H, Chan F F. (1994) Lingual mandibular bone defect. Case report and review of the literature. Aust Dent. 39(6), 368-371.
- 7.Yildirim D, Gormez O, Bozdemir E. (2017) Imaging characteristics of Stafne’s Bone Cavity: Pictorial Essay. , Iran J. Radiol 14(2), 40701.
- 8.Quesada-Gomez C, Valmaseda-Castellon E, Berini-Aytes L. (2006) Stafne bone cavity: a retrospective study of 11 cases. Med Oral Pathol Oral Cir Bucal. 11(3), 277-280.
- 9.Wolf J. (1985) Bone defects in mandibular ramus resembling developmental bone cavity (Stafne). Proc Finn Dent Soc. 81, 215-221.
- 10.Barker G R. (1988) A radiolucency of the ascending ramus of the mandible associated with invested parotid salivary gland material and analogous with a Stafne bone cavity. Br J Oral Maxillofac Surg. 26, 81-84.
- 11.Campos P S, Panella J, Crusoe-Rebello I M, Azevedo R A. (2004) Mandibular ramus-related Stafne bone cavity. Dentomaxillofac Radiol. 33, 63-66.
- 12.Shields E D. (2000) Technical note: Stafne static mandibular bone defect- further expression on the buccal aspect of the ramus. , Am J Phys Anthropol 111, 425-427.
- 13.Kahn J L, Bourjat P, Barriere P. (2002) Ectopic parotid gland in the mandible and masseter muscle. , Rev Stomotol Chir Maxillofac 103, 195-197.
- 14.Ertas E T, Atici M Y, Kalabalik F. (2013) An unusual case of double idiopathic ramus-related Stafne bone cavity. Oral Radiol. 29, 193-197.
- 15.Lee K H, Thiruchelvam J K, McDermott P. (2015) An unusual presentation of Stafne bone cyst. J Maxillofac Oral Surg. 14, 841-844.
- 16.Anbiaee N, Ebrahimi S, Ebrahimnejad H. (2016) Stafne bone defect in the ramus of the mandible: a case report. J Dentomaxillofac Radiol Pathol Surg. 5, 37-41.
- 17.Chen C A, Ahn Y, Odell S. (2016) Developmental salivary gland depression in the ascending mandibular ramus: a cone beam computed tomography study. Imaging Sci Dent. 46, 223-237.
- 18.FB De Araujo Neto, SGB Carneiro, DYA Fugita. (2017) Stafne’s bone defect in atypical location: between the subcondylar region of the neck of the mandible ramus. Open journal of medical imaging. 7, 124-129.
- 19.Hisatomi M, Munhoz L, Asaumi J. (2017) Parotid mandibular bone defect: A case report emphasizing imaging features in plain radiographs and magnetic resonance imaging. Imaging Sci Dent. 47, 269-273.
